NUTRIENT DEFICIENCIES
Definition
What are nutritional deficiencies ?
Etymology helps us learn about nutrient deficiency, with “nutrient” deriving from the Latin verb nutrire, “to nourish” and “deficiency” also owing its roots to the Latin language - deficere - “to be lacking or left wanting”.
In a nutshell, this term describes the state when the body has insufficient levels of one or more nutrients, making the body unable to normally perform its functions".3-5
There are 2 types of nutrients
MACROnutrientS | MICROnutrients |
|---|---|
| Proteins | Minerals: Calcium (Ca), Magnesium (Mg) |
| Carbohydrates | Trace elements: Zinc (Zn), Iron (Fe), Copper (Cu), iodine |
| Lipids | Vitamins: Vit D, Vit C, Vit B |
Today, more than 2 billion people worldwide suffer from vitamin and mineral deficiencies1 .
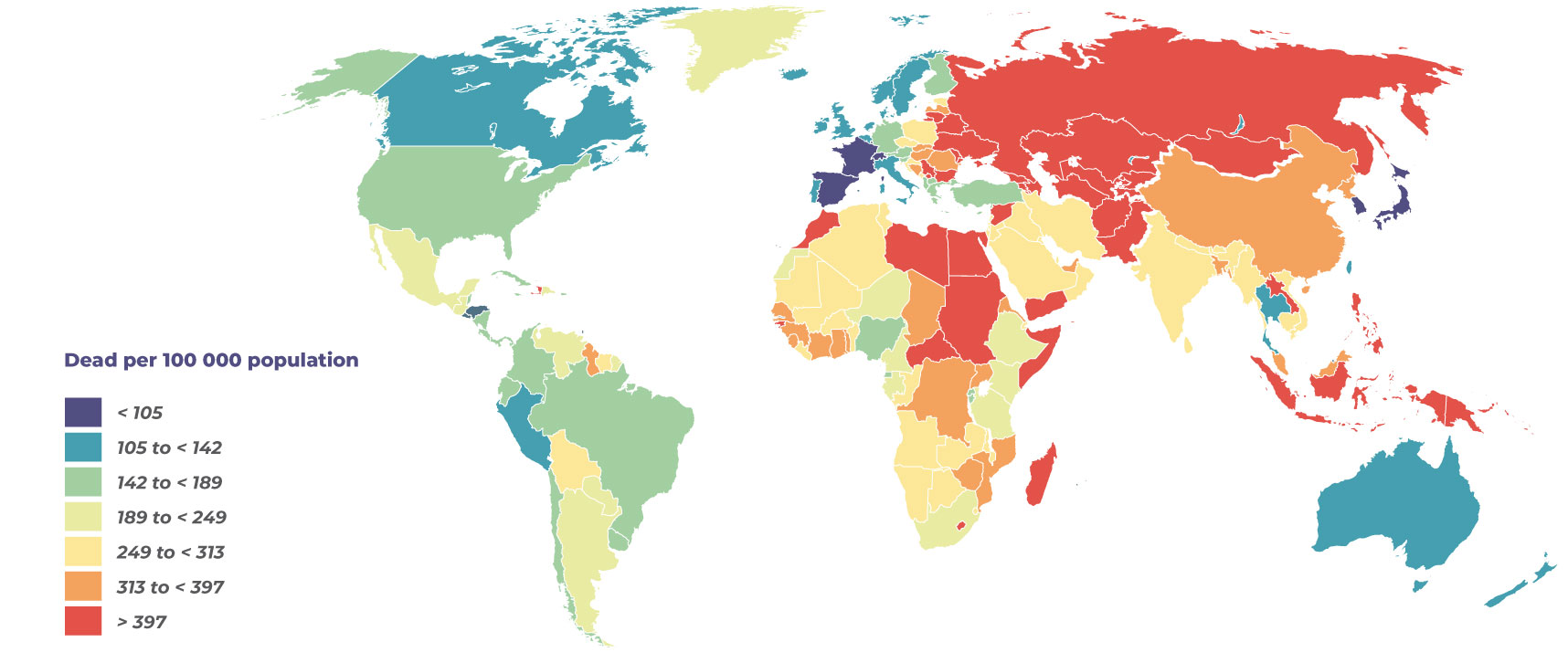
Across the globe, malnutrition was the number one cause of death in 2017 6 .Such dietary deficiency is a public health problem that can induce increasingly common conditions like iron deficiency anemia and osteoporosis7.
MALNUTRITION IS THE NUMBER-ONE CAUSE OF DEATH WORLWILDE (2017)6, 8
11 million deaths and 255 million deaths in terms of disability-adjusted life years.
Risk factors: Top 3 |
|---|
| 1. High sodium diet |
| 2. Whole-grain-deficient diet Iron, Zinc, Vit B1, B2, B6, Folates) |
| 3. Fruit-deficient diet Vit C, Vit A, Folates) |
Causes
What causes nutrient deficiencies ?
Various nutritional deficiencies have multiple causes8:
| Decreased intake | Increased losses | Increased needs |
|---|---|---|
| Malabsorption | Menstrual cycle | Pregnancy |
| Drug/nutrient interactions | Diarrhea | Breastfeeding |
| Monotonous diet | Parasitic infections | Growth periods |
| Low animal food intake | Acute, chronic diseases | |
| Poverty, poor economic status | ||
| Food seasonality | ||
| Food shortages |
Consequences
What are the consequences of these nutritional deficiencies, and related symptoms8?
- Anemia
- Dental disease
- Disorders - cognitive, hepato-digestive, visual, skin conditions
- Cardiovascular disease
- Cancer
- Neural tube defects (NTDs)
- All other birth defects (orofacial cleft palate, heart defects)
- Osteoporosis
- Stunted growth
- Mental delay
- Œdema
Most common nutrient deficiencies
What are the most common nutrient deficiencies?
There are 8 common nutrient deficiencies 5, 9-11:
- Vitamin A - essential for maintaining the integrity of epithelial tissues in the eye, as well as in the urinary, intestinal, and respiratory tracts;
- Folate - crucial for the synthesis of purines and thymidylate, it plays a significant role in DNA synthesis, repair, and stability. It is also involved in carbon metabolism and changes in DNA methylation patterns.
- Iodine - this trace element that plays a major role in thyroid hormone synthesis;
- Zinc - essential for health, associated with cellular metabolism. It is necessary for the proper functioning of over 200 enzymes and is crucial for normal growth and development, immune system function, DNA and protein synthesis, and cell division;
- Vitamin D – essential for the intestinal absorption and metabolism of calcium, magnesium, and phosphorus;
- Iron - major contributor in hemoglobin synthesis;
- Vitamin B12 - required for the development, myelination, and function of the central nervous system; healthy red blood cell formation; and DNA synthesis;
- Calcium - crucial throughout life to maintain bone health.
Iron deficiency (ID) and iron deficiency anemia (IDA)
On the one hand, iron deficiency (ID) refers to a depletion in the body’s total iron content. On the other, iron deficiency anemia (IDA) denotes distinctly low iron levels in our body which are unable to support red blood cell (RBC) production. Of all chronic anemia conditions, it is the most prevalent.
What is anemia ?
Anemia is a common condition affecting 1 in 3 people the world over. It defines a decrease in red blood cells (RBCs), induced by the body’s iron deficiency. Depleted iron levels equal less hemoglobin, meaning fewer and smaller RBCs. Since hemoglobin is the protein that carries oxygen, the body doesn't get all the oxygen it needs13.
Patients at high risk of iron deficiency anemia:
CHILDREN
| Why? The World Health Organization (WHO) reported that toddlers and preschool children have the highest anemia prevalence, representing 42,6% of their demographic, largely owing to nutritional choices. 15 While children require higher iron levels for growth many receive less than their recommended daily intake. In fact, this age group receives a healthy dairy supply, which is deficient in iron, heightening risk of children developing iron-deficiency anemia8. What are the consequences of anemia in children?17, 18, 19
|
|---|---|
WOMAN OF CHILDBEARING AGE
| Why? With a global prevalence of 29.4% for all women of reproductive age and 38.2% for pregnant women, this demographic suffers a higher anemic risk. 15 This is due to blood loss experienced in menstruation and increased blood pressure required for foetal development during pregnancy.20, 21. Women of childbearing age represent the most at-risk demographic for contracting iron deficiency anemia (IDA). The WHO 22 estimates that 496 million are non-pregnant women.
What are the consequences of anemia in women of childbearing age? Whilst this population segment is vulnerable to iron deficiency anemia, pregnant women run a greater risk due to high iron requirements. Pregnant women with IDA can experience23, 24
|
SURGERY PATIENTS | Why? The mean prevalence of pre-operative anemia is around 35%26. The aetiology of pre-operative anemia may be multifactorial and complex (nutritional deficiencies, specific drugs, immune system activation). The mean prevalence of post-operative anemia can reach 90%, mainly induced by pre-operative anemia and important blood loss during surgery.25 What are the consequences of anemia in surgical patients? |
ELDERLY | Why? Anemia is common in the elderly, its prevalence increasing with age. The second most frequent cause among the elderly, iron deficiency anemia is typically triggered chronic gastrointestinal blood loss, in turn caused by nonsteroidal anti-inflammatory drug–induced gastritis, ulcers, colon cancer, diverticula and angiodysplasia. Generally, older persons lack iron intake and absorption.27 What are the consequences of anaemia in elderly patients? |
VEGETARIANS | Why? Because of vegetarians’ diet, which is low in nutrient deficiency, notably animal foods – a requisite source of iron.29 How? The poor bioavailabilty of nutrients induces anemia since vegetarians’ recommended daily intake of iron is 1.8 times higher than those who eat meat.30 |
ATHLETES | Why? The intensity of elite-level sports calls for increased iron demand, in turn accelerating low iron levels. How? Anemia therefore results from athletes’ elevated iron loss, which in turn, blocks iron absorption caused by hepcidin bursts.31 |
What are symptoms of iron deficiency anemia?32-36
- Fatigue
- Difficulty in concentrating
- Dizziness or lightheadedness
- Cold hands and feet
- Pale skin
- Dyspnea on exertion
- Brittle nails
- Hair loss
How do you treat anemia?
Anemia treatment depends on two factors; severity and its underlying cause. 14
IRON SUPPLEMENTS | DIETARY CHANGES |
|---|---|
| Generally, IDA treatment will include iron supplements and lifestyle changes to remedy symptoms by increasing iron. Adults should discuss dietary benefits with a health professional. | Certain foods are iron-rich and need encouraging 37
|
Which foods should be avoided if one is anemic?
Other food and drinks display low iron levels, with deficient absorption (avoid in large quantities) 38.
- Tea39.
- Coffee.
- Dairy products.
- Foods with high levels of phytic acid - wholegrain cereals.
Calcium & Vitamin D deficiencies
Common nutritional deficiencies, also concern calcium and vitamin D. Both types of nutrient deficiency are on the rise: according to the US Department of Agriculture (USDA), close to 30 % of men and 60 % of women older than age 19 years do not consume enough calcium, and more than 90 % of Americans do not consume enough vitamin D40.
Why are calcium and vitamin D of significance ?
- The benefits of Vitamin D include bone mineralization and calcium absorption from the intestine.
- As a micronutrient, calcium fortifies the body (bones).
Calcium also involves metabolism, via blood clotting, cell adhesion, muscle contraction, hormone neurotransmitter release, glycogen metabolism, and cell proliferation and differentiation. 8, 41
Which disease is caused by a calcium and vitamin D deficiency ?
Nutrient deficiency in vitamin D and calcium terms can cause skeletal problems, manifested as rickets (children) and osteoporosis (adults). 8
Who is at high risk? 8, 41-44:
YOUNG PEOPLECHILDREN AND ADOLESCENTS 42
| Why? Childhood and adolescence are key skeletal formation stages, requiring increased calcium intake. However, many young people do not eat a traditional, calcium-rich breakfast. Low levels of vitamin D in children have been reported in studies worldwide, with the cause attributed to indoor lifestyle, urban pollution and even sunscreen. Which consequences? Although rare in industrialized countries, children with severe vitamin D deficiency experience growth retardation, low bone density and deformities. Bones that are not healthy during youth are more prone to result in an increased susceptibility to osteoporosis and fractures in later life and tend to suffer from increased osteoporosis. |
MENOPAUSALWOMEN DURING OR POST MENOPAUSAL PERIOD 43
| Why? Estrogen health key to regulating bone turnover throughout life. However, as women become estrogen-deficient when menses cease, bone resorption exceeds bone formation, decreasing calcium intestinal absorption and kidney retention. Which consequences? Did you know? One in three women aged over 50 suffers a skeletal fracture caused by osteoporosis. |
ELDERLYTHE ELDERLY 43, 44
| Why? More often than not, the elderly:
Which consequences? Osteoporosis inflicts pain, long-term disability and loss of independence among older adults, potentially inducing premature death. |
What are the long-term risks and associated signs of a severe vitamine d deficiency and calcium imbalance? What are the associated signs or symptoms?41, 43
- Increased fractures
- Exacerbated development or worsening of skeletal disorders -: rickets, osteomalacia.
- Stunted growth.
- Osteoporosis.
There are often no clear symptoms of vitamin D and calcium deficiencies, except in more severe cases.
How do tou treat vitamin D and calcium deficiency?
RESPONSIBLE SUN EXPOSURE
Our skin produces vitamin D from the sun’s rays (UVB irradiation), the main “free” source
However sunlight is not the most reliable nutrient deficiency remedy due to its related risk of skin aging and cancer.41
DIETARY CHANGES
Calcium | Vitamin D |
|---|---|
|
|
Gentle reminder
Your expert dieticians can assist you in determining your body's calcium & vitamin D needs.
References
- Kant AK. Consumption of energy-dense, nutrient-poor foods by adult Americans: nutritional and health implications. The Third National Health and Nutrition Examination Survey, 1988-1994. Am J Clin Nutr. 2000;72(4):929-936.
- Marriott BP, Olsho L, Hadden L, Connor P. Intake of added sugars and selected nutrients in the United States, National Health and Nutrition Examination Survey (NHANES) 2003-2006. Crit Rev Food Sci Nutr. 2010;50(3):228-258.
- Nutrient. Merriam Webster. Accessed on April 23th 2024.
- “Deficient.” Merriam-Webster.com Dictionary, Merriam-Webster, https://www.merriam-webster.com/dictionary/deficient. Accessed April 23th 2024.
- Kiani AK, Dhuli K, Donato K, Aquilanti B, Velluti V, Matera G, Iaconelli A, Connelly ST, Bellinato F, Gisondi P, Bertelli M. Main nutritional deficiencies. J Prev Med Hyg. 2022 Oct 17;63(2 Suppl 3):E93-E101. doi: 10.15167/2421-4248/jpmh2022.63.2S3.2752. PMID: 36479498; PMCID: PMC9710417.
- Afshin, A., Sur, P.J., Fay, K.A., Cornaby, L., Ferrara, G., Salama, J.S., Mullany, E.C., Abate, K.H., Abbafati, C., Abebe, Z., et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 0. (2019).
- Anuraj H Shankar. Mineral Deficiencies. Hunter’s Tropical Medicine and Emerging Infectious Disease (Ninth Edition) 2013, Pages 1003-1010.
- Lindsay A. et al. Guidelines on food fortification with micronutrients. WHO Library Cataloguing-in-Publication Data. 2006. 3-86.
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B(6), Folate, Vitamin B(12), Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academies Press; 1998.
- Allen LH. Vitamin B-12. Adv Nutr 2012;3:54-5. [PubMed abstract]
- Stabler SP. Vitamin B12. In: Marriott BP, Birt DF, Stallings VA, Yates AA, eds. Present Knowledge in Nutrition. 11th ed. Washington, DC: Elsevier; 2020:257-71.
- Bermejo F, García-López S. A guide to diagnosis of iron deficiency and iron deficiency anemia in digestive diseases. World J Gastroenterol. 2009 Oct 7;15(37):4638-43. doi: 10.3748/wjg.15.4638. PMID: 19787826; PMCID: PMC2754511.
- Nicholas JK. et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014.123: 615–24.
- Lopez A et al. Iron deficiency anaemia. Lancet. 2016 Feb 27;387(10021):907-16
- WHO Library Cataloguing-in-Publication Data 2015. The global prevalence of anaemia in 2011.
- Munoz M et al.‘Fit to fly’: overcoming barriers to preoperative haemoglobin optimization in surgical patients. British Journal of Anaesthesia. 2015; 115 (1): 15–24.
- Bandhu R et al. Effect of iron on growth in iron deficient anemic school going children. Indian Journal of Physiology and Pharmacology. 2003. 47 (1) : 59-66.
- Grantham-McGregor S et al. A Review of Studies on the Effect of Iron Deficiency on Cognitive Development in Children. J Nutr. 2001 Feb;131(2S-2):649S-666S.
- Ekiz C et al. The effect of iron deficiency anemia on the function of the immune system. The Hematology Journal. 2005. 5: 579-583.
- World Health Organization. Iron, In: Vitamin and mineral requirements in human nutrition. Second edition. 2005: 246-78. (p 264,266)
- Galan P et al. Determining factors in the iron status of adult women in the SU.VI.MAX study. Eur J Clin Nutr 1998; 52: 383-8.
- Iron Deficiency Anaemia: Assessment, Prevention and Control. A Guide For Programme Managers (Document WHO/NHD/01.3). Geneva: World Health Organization, 2001 https://www.who.int/publications/m/item/iron-children-6to23--archived-iron-deficiency-anaemia-assessment-prevention-and-control
- Vural T et al. Can anemia predict perinatal outcomes in different stages of pregnancy? Pakistan Journal of Medical Science. 2016. 32(6) : 1354-1359.
- Huch R et al. Iron Deficiency and Iron Deficiency Anemia. Pocket Atlas Special. Thieme. 2006. Chapter 4 : 34-38
- Muñoz , M., Franchini , M., and Liumbruno , G.M. (2018). The post operative management of anaemia: more efforts are needed. Blood Transfus 16, 324 325.
- Muñoz, M., Gómez Ramírez , S., Campos, A., Ruiz, J., and Liumbruno , G.M. (2015). Pre operative anaemia: prevalence, consequences and approaches to management. Blood Transfus. Trasfus . Sangue 13, 370 379.,).
- Smith DL. Anemia in the Elderly. Am Fam Physician. 2000 Oct 1;62(7):1565-1572
- Maerevoet, M., Sattar, L., Bron, D., Gulbis, B., and Pepersack, T. (2014). [Anemia in the elderly]. Rev Med Brux 35, 361–367
- Institute of Medicine (US) Panel on Micronutrients. Washington (DC): National Academies Press (US) (2001).
- Pawlak R, Berger J, Hines I. Iron Status of Vegetarian Adults: A Review of Literature. Am J Lifestyle Med. 2016 Dec 16;12(6):486-498. doi: 10.1177/1559827616682933. PMID: 30783404; PMCID: PMC6367879.
- Clénin G, et al. Swiss Med Wkly. 145, w14196 (2015).
- Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372(19):1832-43.
- National Heart, Lung, and Blood Institute website. Iron-deficiency anemia. www.nhlbi.nih.gov/health-topics/iron-deficiency-anemia. Updated 18 April 2023. Accessed 31 October Sit2023.
- Killip S, Bennett JM, Chambers MD. Iron deficiency anemia. Am Fam Physician. 2007;75(5):671-8.
- Auerbach M, Adamson JW. How we diagnose and treat iron deficiency anemia. Am J Hematol. 2016;91(1):31-8.
- Camaschella C. Iron deficiency. Blood. 2019;133(1):30-9.
- Les références nutritionnelles en vitamines et minéraux | Anses - Agence nationale de sécurité sanitaire de l’alimentation, de l’environnement et du travail https://www.anses.fr/fr/content/les-r%C3%A9f%C3%A9rences-nutritionnelles-en-vitamines-et-min%C3%A9raux
- Lesjak M et al. Role of dietary flavonoids in iron homeostasis. Pharmaceuticals 2019, 12, 119; doi:10.3390/ph12030119.
- Thankachan P, Walczyk T, Muthayya S, et al. Iron absorption in young Indian women: the interaction of iron status with the influence of tea and ascorbic acid. The American Journal of Clinical Nutrition. 2008;87(4):881-886. doi: 10.1093/ajcn/87.4.881
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020.
- Heike A. Bischoff-Ferrari. THREE STEPS TO UNBREAKABLE BONES, VITAMIN D, CALCIUM AND EXERCISE. International Osteoporosis Fondation. World Osteoporosis Day 2011.
- Bess Dawson-Hughes, Ghada El-Hajj Fuleijan & Patricia Clark. Building strong bones in children and adolescents. International Osteoporosis Fondation. World Osteoporosis Day 2013.
- Cyrus Cooper, Bess Dawson-Hughes, Catherine M. Gordon, René Rizzoli. Healthy Nutrition, Healthy Bones. International Osteoporosis Fondation. World Osteoporosis Day 2015.
- Lanier JB, et al. Am Fam Physician. 98, 437-442 (2018).