VENOUS DISEASE
Venous disease encompasses a variety of conditions that affect the veins, which are blood vessels responsible for returning deoxygenated blood back to the heart. When the veins in the body cannot effectively return blood to the heart, it can lead to several venous disorders.
In everyday life, venous disease can lead to signs and symptoms that vary depending on the severity and type of venous disease, but common symptoms include heavy legs, swelling, itching, and pain 1
This condition raises several important questions which we explore in this article:
- What are these venous diseases?
- What are their symptoms?
- What exactly is the primary cause?
- What are the treatment options?
Various venous diseases
Venous diseases indicate every venous disorder created from infected, abnormal or malfunctioning veins.
Venous diseases can affect different parts of the body: legs (varicose veins), rectum (hemorrhoids), abdomen (pelvic congestion syndrome).
The most commun venous disases are :
Varicose veins and Chronic Venous Insufficiency (CVI)
Did you know ?
About 35% of the global population experience early stages of Chronic Venous Disease2.
Venous return refers to the flow of deoxygenated blood from the body's tissues back to the heart.
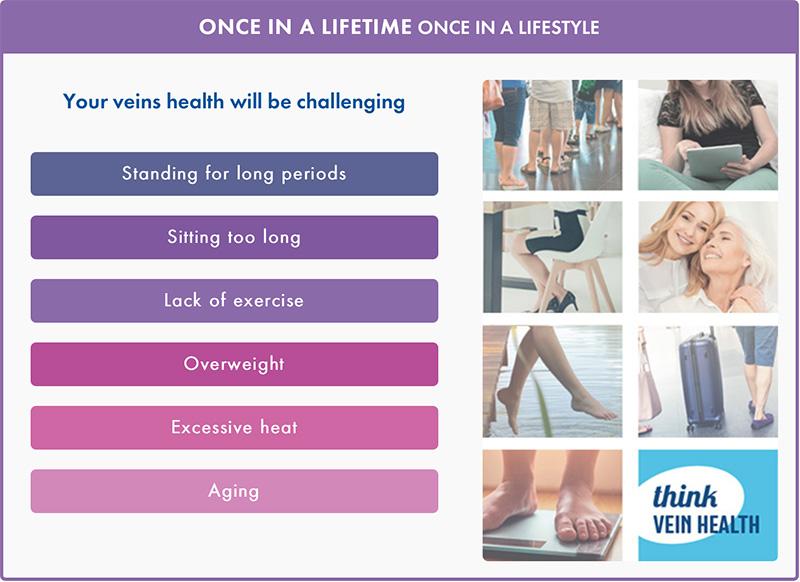
Venous disease can be triggered by factors such as genetics, aging, and prolonged periods of standing or sitting. Obesity, pregnancy, and hormonal changes also contribute to the risk. Additionally, lack of physical activity, injury, smoking, and blood clots can lead to the onset of various forms of venous disease3.
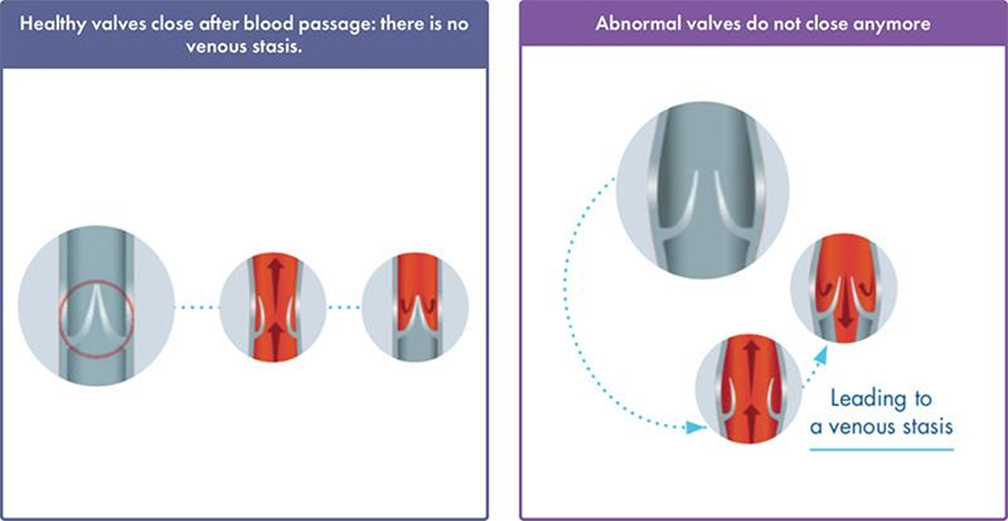
Venous disease involves the malfunctioning of the veins, particularly the venous valves.
Venous valves are small flaps within the veins that open and close to help blood move towards the heart. They prevent the backward flow of blood, ensuring a one-way system.
When valves become weak or damaged, they do not close properly, making it difficult for blood to flow through vein walls and back to the heart. This is called Venous Insufficiency.
Chronic Venous Insufficiency can lead to varicose veins, which are swollen, twisted veins that lie just under the skin. They usually occur in the legs. This is the first stage of Chronic Venous Disease.
People with Chronic Venous Disease may present heaviness, tired legs, feelings of swelling, itching of the skin, nocturnal cramps, throbbing, burning pain, aching of the legs, which is exacerbated by prolonged standing or sitting, or difficulties during exercise3.
What is the most common cause of Chronic Venous Disease ?
The most common cause of Chronic Venous Disease are: 3;4
Many established risk factors are involved in CVD, especially age, excess weight, heredity, occupations associated with orthostasis. CVD prevalence has been shown to be higher in a population with family history of the disease.
Not dissimilar to sedentary habits, i.e., any behavior characterized by a low energy expenditure (≤ 1.5 kcal/kg/hour), while in a sitting, reclining, or lying posture, chronic venous disease is induced by the following risk factors:
Prolonged sitting/standing
Sedentary lifestyle
Obesity
Excessive heat
Age (veins gradually contract less easily)
Pregnancy with the heightened risk of varicose veins and deep vein thrombosis.
Family history and genetics
Thromboembolic disorders
High heels
Venous disorders often present comorbidities which can be 5:
- Type 2 diabetes,
- Arterial hypertension,
- Heart failure,
- Joint leg diseases,
- Inflammatory bowel disease,
- Renal insufficiency,
- Pulmonary diseases
- Malignant disease.
Chronic Venous Disease Symptoms
What symptoms do patients experience1;3?
Patients' symptoms are the leading cause of clinical consultation in vascular medicine, experienced in early Chronic Venous Disease stages.
Heavy legs with pain
Swelling in the legs
Night cramps
Other symptoms include:
Sensations of 'pins and needles', burning and tightness in the legs
Itching in the legs, with or without visible cutaneous ulcers
Grogginess and fatigue
Restless legs syndrome (RLS)
Symptoms are most felt in the lower calves and tend to increase
As the day goes on and during hot weather
After prolonged sitting/standing
At the end of the day and/or nighttime
These symptoms can indicate conditions other than venous disease, but their absence does not exclude Chronic Venous Disease.
Diagnosis
Diagnosis is made by combining a visual examination of the legs and patients’ symptoms6.
Your doctor must also perform a Doppler or Duplex Ultrasound to determine venous reflux and/or obstruction as well as the severity.
The CEAP classification (Clinical-Etiology-Anatomy-Pathophysiology) will help categorize chronic venous insufficiency, which is heterogenous among patients. The Clinical aspect ranges from C0 (no clinical sign) to C6 (open ulcer) based on disease severity.
Categorizing the condition of your legs:
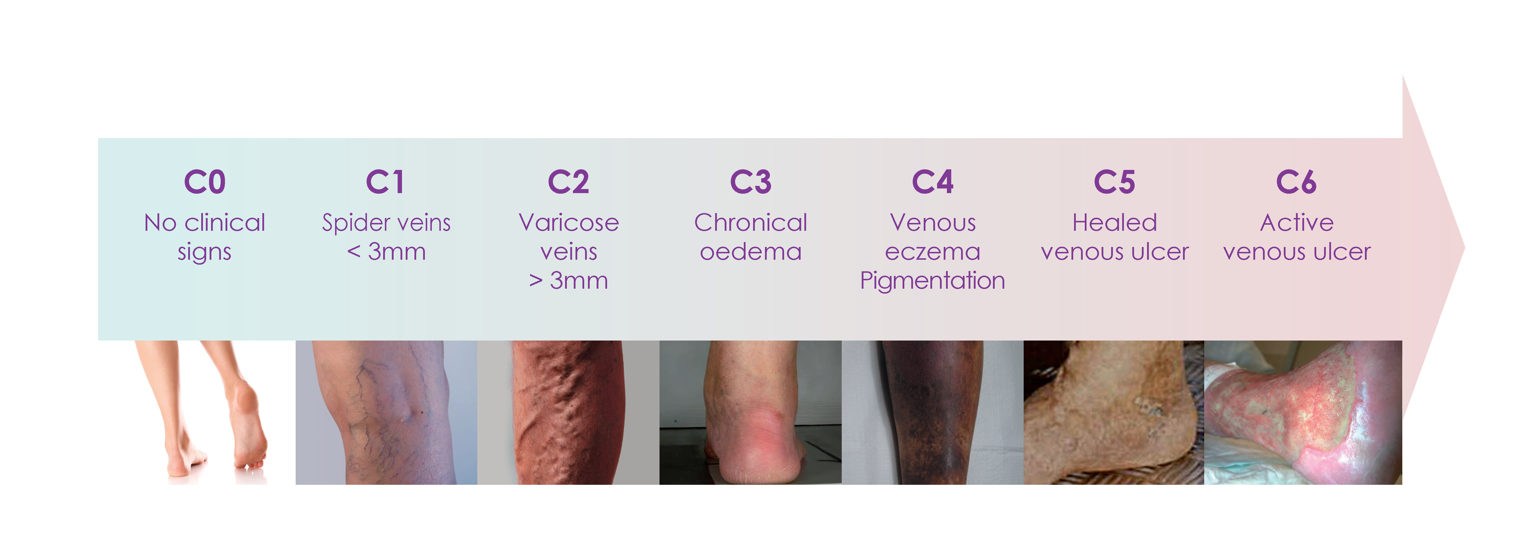
Chronic Venous Insufficiency conditions can manifest from spider veins (reticular veins) to leg ulcers. It is considered an established CVD from the emergence of varicose veins.
Evolution of the pathology
Venous stasis - when blood pools in the veins - poses the risk of developing venous thrombosis, which can be of serious concern.
Deep vein thrombosis (DVT) is the detection of a blood clot in the deep veins, occurring mostly in the legs. It includes limb swelling, pain, discoloration, itching, and ulcer formation.
A more dramatic scenario is when the blood clot moves up from deep veins in the legs to obstruct the pulmonary artery thus causing pulmonary embolism. The latter is one of the major causes of mortality worldwide.
Prevention of DVT thereby decreases the incidence of a pulmonary embolism7.
What are the treatment options ?
There is a local and systemic approach to CVD. Always remember to preapare thoroughly and consult your doctor before starting treatment6.
VENOACTIVE DRUGS | COMPRESSION STOCKINGS | VARICOSE VEINS REMOVAL SURGERY |
|---|---|---|
| Patients with persisting leg symptoms of chronic venous disease before or after surgery of varicose veins should consider to use the right venoactive drug. | Compression stockings apply pressure to the legs, reducing venous reflux and restoring blood flow to the heart. Ultimately, pressure depends on the disease stage. These stockings alleviate functional symptoms, considerably improving patients’ quality of life. They also prove essential in the latter disease stages, e.g., edema and skin ulcers. Compression stockings are available in different formats and can be used during pregnancy. | Until recently, traditional vein ligations – with or without stripping – had been the gold standard for varicose vein treatment. Despite good outcomes, surgery is not devoid of adverse effects (ecchymosis, hematoma, tenderness, infection, etc.). Less invasive treatments for varicose veins include sclerotherapy, endovenous laser ablation (EVLA) and radio-frequency ablation (RFA). |
Anorectal veins: Hemorrhoidal disease
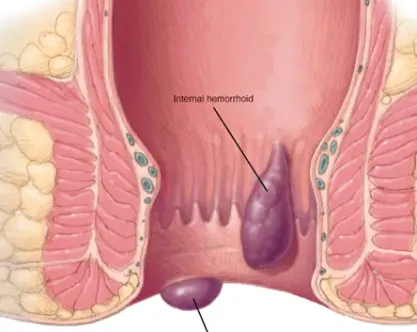
Hemorrhoids are cushions of highly vascular tissue, located at the anal canal of all healthy individuals 8.
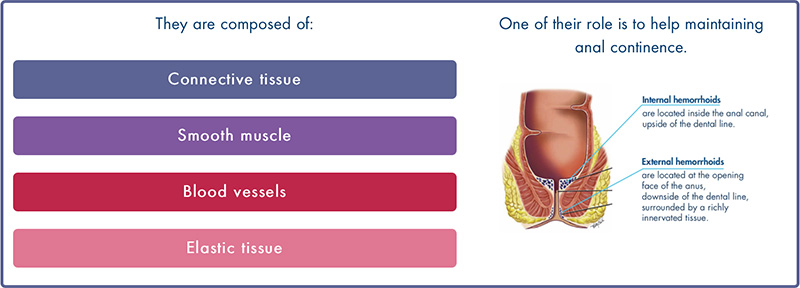
Although normal structures, the term “hemorrhoids” is now associated with the pathological conditions known as “hemorrhoidal disease” or “hemorrhoidal crisis.”
What is hemorrhoidal disease?
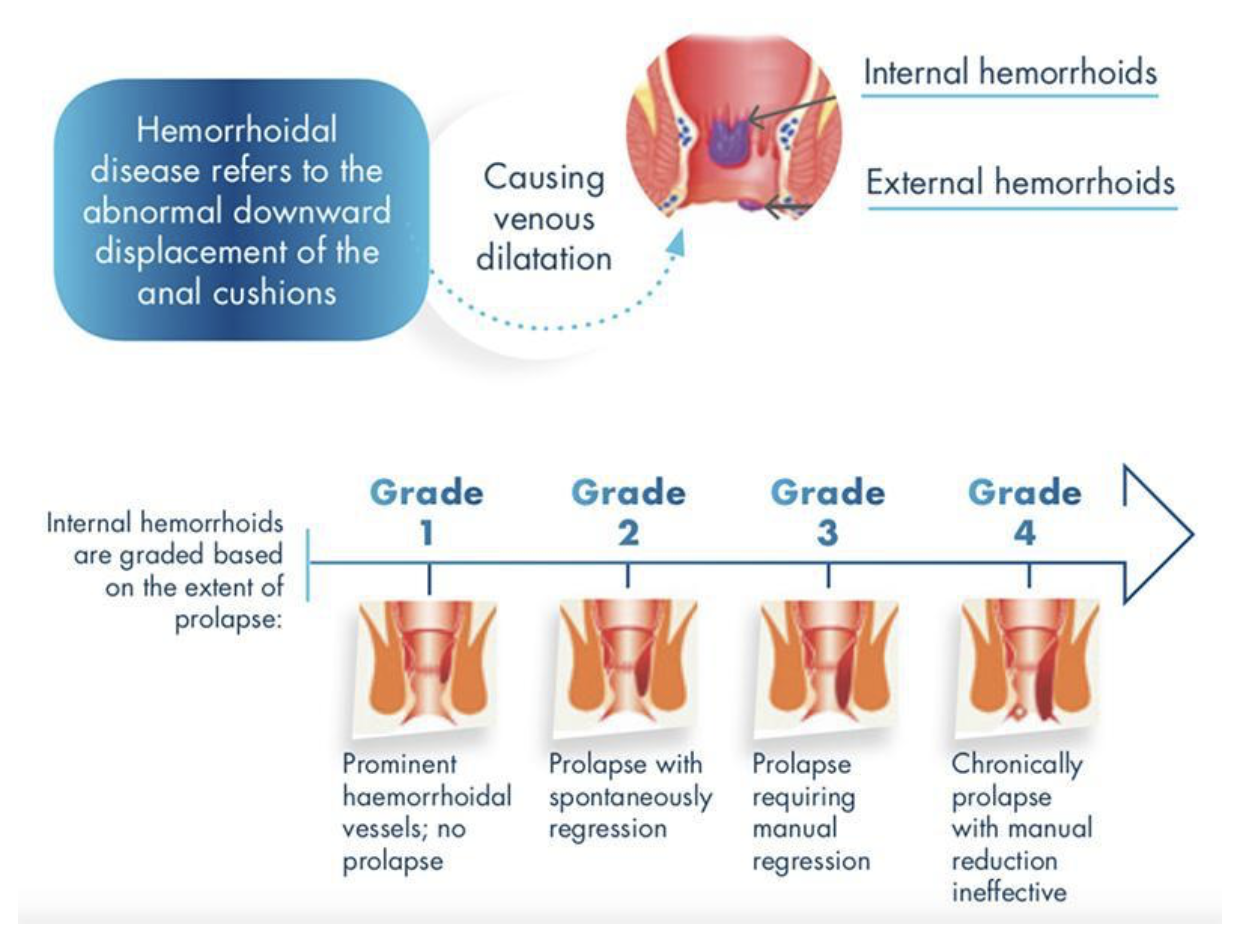
Hemorrhoidal disease8 is a type of varicose vein occurring in the rectum and anus, causing itching, bleeding, and pain during bowel movements. Hemorrhoidal disease development is still poorly understood.
Nowadays, the origin of hemorrhoidal disease is considered to be local tissue deterioration.
What causes hemorrhoidal disease?
Hemorrhoids’ risk factors include9:
- Obesity
- Prolonged defecating /sitting
- Increased abdominal pressure - heavy lifting
- Insufficient intake of dietary fibers and oral fluids
- Transit dysregulation - constipation, chronic diarrhea
- Family history and genetics
- Pregnancy
- Aging
- Local impairment - anal intercourse, rectal pathology
- Straining for defecation
- Alcohol, fatty and spicy foods
Since prolonged physical inactivity promotes constipation, it is also a risk factor of hemorrhoidal disease.
Hemorrhoids symptoms
The symptoms8 of hemorrhoids depend on the type you have.
If you have extenal hemorrhoids, you may have :
- Anal itching
- One or more hard, tender lumps near your anus, anal ache or pain, especially when sitting.
Too much straining, rubbing, or cleaning around your anus may make your symptoms worse. For many people, the symptoms of external hemorrhoids go away within a few days.
If you have internal hemorrhoids, you may have:
- Bleeding from your rectum ––bright red blood in your stools, on toilet paper, or in the toilet bowl after a bowel movement
- A hemorrhoid that has fallen through your anal opening, called prolapse
Internal hemorrhoids that are not prolapsed most often are not painful. Prolapsed internal hemorrhoids may cause pain and discomfort.

Hemorrhoidal disease is not considered as serious condition, but its symptoms can affect the quality of life or interfere with daily activities.
Diagnosis
The most common presentation of hemorrhoidal disease is painless rectal bleeding during defecation with or without prolapse. The blood is bright red and normally on the outer surface of stool. The blood can also be seen during cleansing.
However, during a hemorrhoidal crisis, severe anal pain may be felt. A precise history and thorough physical examination, including digital rectal examination and anoscopy, are imperative for the diagnosis of hemorrhoids.
Unless bright red blood is clearly seen from hemorrhoids, if you have rectal bleeding, you should talk about it to your doctor immediately, they may then schedule a colonoscopy to exclude more serious conditions10.
How do I know if I have hemorrhoidal disease?
All symptoms of hemorrhoids are non-specific, with other conditions concomitantly present and causes of similar signs (anal fissure, malignancy, inflammatory bowel diseases, etc.).
This calls for questioning and comprehensive diagnosis:
- External inspection
- Digital examination
- Further tests
See a doctor immediately if you have blood in your stools. This can indicate hemorrhoids, but also a more serious condition.
What are the complications of Hemorrhoidal disease?
The complications of Hemorrhoidal disease are9:
- Anemia
- Blood clots in external hemorrhoids
- Infection
- Skin tags (flap of tissue that hangs off skin)
- Strangulated hemorrhoids (muscles in the anus cut off blood flow to a prolapsed internal hemorrhoid).
What are the treatment options?
TREATMENT METHODS10
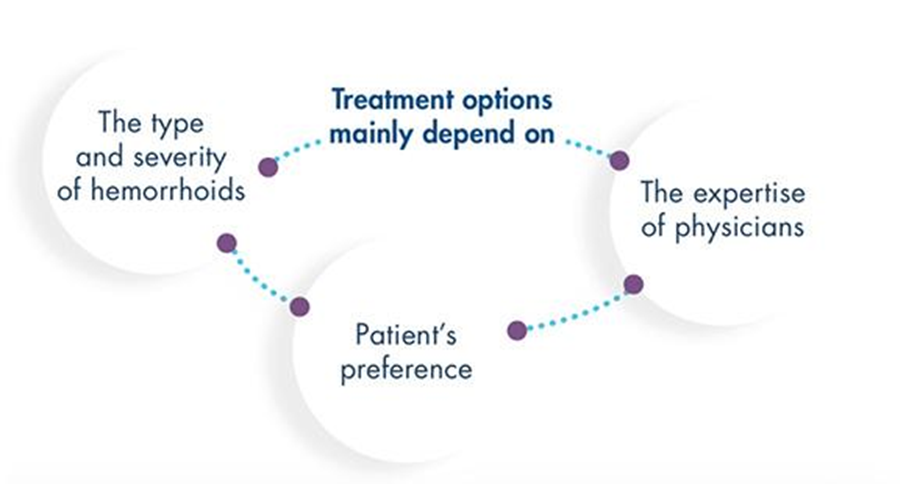
LIFESTYLE AND DIETARY CHOICES
Purpose: to prevent/reduce the pathological development or symptoms of hemorrhoidal disease.
Examples include regular exercise, zero anal intercourse and reduced alcohol consumption
Transit regulation is critical to your body. Remember to prepare your questions and visit the doctor before administering treatment.
INSTRUMENTAL AND SURGICAL TREATMENT
Purpose: to induce fibrotic scarring of internal hemorrhoids.
Examples include rubber band ligation and infrared coagulation.
Despite the range of technical surgery, it is restricted to severe cases of hemorrhoids.
PHARMACOLOGICAL TREATMENT
Purpose: to relieve symptoms.
- Intestinal transit modifiers help regulate stool frequency
- Non-steroidal anti-inflammatory drugs (NSAIDS), analgesics, and cortisone derivatives can be used in case of pain caused by thrombosed hemorrhoids. However, they should be used carefully for safety reasons.
- Another option is localized topical treatments (suppositories, creams, ointments) combining applied corticosteroids, anesthetics, lubricants, protectors and phlebotonics.
- Sitz baths also reduce hemorrhoidal pain.
- Specific medication must be carefully administered to pregnant women.
Hemorrhoidal disease in pregnant women and other patient types/ demographics
Pregnancy and delivery predispose women to develop hemorrhoids because of hormonal changes and increased intra-abdominal pressure. It has been estimated that 25% to 35% of pregnant women are affected by this condition. In certain populations, up to 85% of pregnancies are affected by hemorrhoids in the third trimester.
What’s more, and unsurprisingly, age is a compounding factor, not to mention adults with obesity, strained bowel movements and those suffering from alcoholism11.
Abdomen: Pelvic congestion syndrome
Pelvic venous insufficiency may cause pelvic venous disorders, which can manifest through many/multiple different signs and symptoms including a Pelvic Congestion Syndrome (PCS). For example, chronic pelvic pain (CPP) is characterized as more than six months of persistent or intermittent pain localized in the pelvis. CPP may be caused by a PCS in up to 30% of women.12
Prevention
How to prevent Venous Diseases?
Physical activity is vital, whether it’s walking just a few steps or biking and swimming which will further reactivate the venous pump function.
Finally, everyday practices can relieve stasis e.g., avoiding tight clothes and high heels and making sure to stand and sit at regular intervals4.
Physical inactivity
What is physical activity? 13 ; 14
Physical activity is defined as any bodily movement produced by the contraction of skeletal muscle that increases energy expenditure above the resting metabolic rate.
MODERATE-INTENSITY | VIGORОUS-INTENSITY | MUSCLE-STRENGTHENING |
|---|---|---|
Moderate-intensity physical activities require some effort, but you can still speak easily while doing these activities :
| Vigorous-intensity physical activities require more effort, making you breathe harder and faster :
| Muscle-strengthening activities cause the body’s muscles to work or resist an applied force or weight :
|
Physical activity guidelines
Describe the amount and types of physical activity that offer substantial health benefits.
The WHO (World Health Organization) recommends that each adult aged 18-64 should accumulate at least.

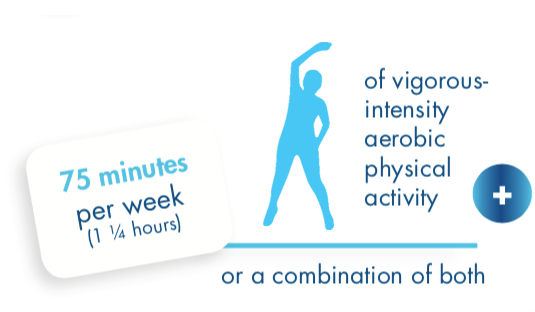

Practical advices
Physical activity needs to be a regular permanent habit. There are many ways to notch up the total of 150 minutes per week of moderate-intensity physical activity.
MOVE MORE…
- Do what you can, some physical activity is better than none!
- Integrate physical activity into your daily routine: spread it throughout the week.
- Start slowly if you have been inactive for a long time and gradually build up the amounts.
- Speak with your doctor or a health professional if you're unsure about your health or how active to be.
- Wear appropriate clothing and footwear, eat well and drink enough water.
… SIT LESS!
- Plan your physical activity. Make a regular time for it in your diary.
- Set some realistic and reachable goals and break into smaller ones.
- Track your progress using step-counting devices (e.g. podometer) or any other apps (e.g. Map my walk/hike/ride under armour) to motivate yourself.
Physical activity practical advices
Along your route
|
|
At work
|
|
Active and fun
|
|
Why should we follow the World Health Organization recommandations?
Having a regular moderate-to-vigorous physical activity as recommended by the WHO 13 can:
- Reduce the risk of:
- All-cause mortality by 33%;
- Cardiovascular disease;
- Type 2 diabetes and help control blood glucose;
- Developing some cancers.
- Maintain or improve blood pressure.
- Help prevent unhealthy weight gain over time.
- Slow the decline in bone density and the loss of muscles.
- Reduce feelings of anxiety.
References
- Bergan, John J et al. “Chronic venous disease.” The New England journal of medicine vol. 355,5 (2006): 488-98. doi:10.1056/NEJMra055289
- Salim, Safa et al. “Global Epidemiology of Chronic Venous Disease: A Systematic Review With Pooled Prevalence Analysis.” Annals of surgery vol. 274,6 (2021): 971-976. doi:10.1097/SLA.0000000000004631
- Ortega, Miguel A et al. “Understanding Chronic Venous Disease: A Critical Overview of Its Pathophysiology and Medical Management.” Journal of clinical medicine vol. 10,15 3239. 22 Jul. 2021, doi:10.3390/jcm10153239
- Glauser F, Codreanu A, Tribout B, Depairon M. Prévention de la maladie veineusechronique : quels conseils donner à nos patients ? Rev Med Suisse. 2012;327: 306–310.
- Davies AH. The Seriousness of Chronic Venous Disease: A Review of Real-World Evidence. Adv Ther. 2019 Mar;36(Suppl 1):5-12. doi: 10.1007/s12325-019-0881-7. Epub 2019 Feb 13. PMID: 30758738; PMCID: PMC6824448.
- De Maeseneer, Marianne G et al. “Editor's Choice - European Society for Vascular Surgery (ESVS) 2022 Clinical Practice Guidelines on the Management of Chronic Venous Disease of the Lower Limbs.” European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery vol. 63,2 (2022): 184-267. doi:10.1016/j.ejvs.2021.12.024
- Chang SL, et al. Association of Varicose Veins With Incident Venous Thromboembolism and Peripheral Artery Disease. Jama. 2018;319(8):807-817.
- Sanchez, Caroline, and Bertram T Chinn. “Hemorrhoids.” Clinics in colon and rectal surgery vol. 24,1 (2011): 5-13. doi:10.1055/s-0031-1272818
- Lohsiriwat V. Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol. 2012 May 7;18(17):2009-17. doi: 10.3748/wjg.v18.i17.2009. PMID: 22563187; PMCID: PMC3342598.
- van Tol, R R et al. “European Society of ColoProctology: guideline for haemorrhoidal disease.” Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland vol. 22,6 (2020): 650-662. doi:10.1111/codi.14975
- Staroselsky, Arthur et al. “Hemorrhoids in pregnancy.” Canadian family physician Medecin de famille canadien vol. 54,2 (2008): 189-90.
- Quaghebeur, Jörgen, and Jean-Jacques Wyndaele. “Chronic pelvic pain syndrome: role of a thorough clinical assessment.” Scandinavian journal of urology vol. 49,2 (2015): 81-9. doi:10.3109/21681805.2014.961546
- World Health Organization. “Physical Activity.” World Health Organization, 26 june 2024, https://www.who.int/news-room/fact-sheets/detail/physical-activity.
- Thivel D, Tremblay A, Genin PM, Panahi S, Rivièere D, Duclos M. Physical activity, inactivity,and sedentary behaviors: definitions and implications in occupational health. Front Public Health. 2018;6: 288.